Health Law: Regulations And Principles In Healthcare
Regulations and Principles in Healthcare is a specialized legal field that focuses on the regulatory framework and principles governing healthcare in the United States. Health Law encompasses a wide range of legal issues, including medical malpractice, healthcare regulation, patient rights, healthcare insurance, and bioethics.
Health law is of paramount importance as it establishes the legal and ethical guidelines for healthcare delivery, safeguarding patient rights, ensuring quality and safety, and addressing public health concerns. Health law benefits society by protecting patients, setting standards for healthcare quality, enabling regulatory oversight, and providing a framework for ethical decision-making in healthcare.
Healthcare lawyers, known as health lawyers, are central to the field. They serve as legal counselors, advising healthcare providers and institutions on compliance with healthcare laws and regulations. These lawyers engage in litigation, representing clients in healthcare-related cases such as medical malpractice and regulatory enforcement actions. Healthcare lawyers participate in policy advocacy, working with government agencies, advocacy groups, and associations like the American Health Lawyers Association (AHLA) to shape healthcare policies and legislation.
Healthcare lawyers play a crucial role in contract negotiation to ensure legal and ethical compliance and address complex ethical issues in healthcare, such as research ethics and end-of-life decisions. Health law and healthcare lawyers are indispensable components of the healthcare system, ensuring its integrity and the well-being of all stakeholders involved.
Table of Contents
- What Is Health Law?
- What Is The Importance Of Health Laws?
- What Are The Benefits Of Health Law?
- What Do Healthcare Lawyers Do?
What Is Health Law?
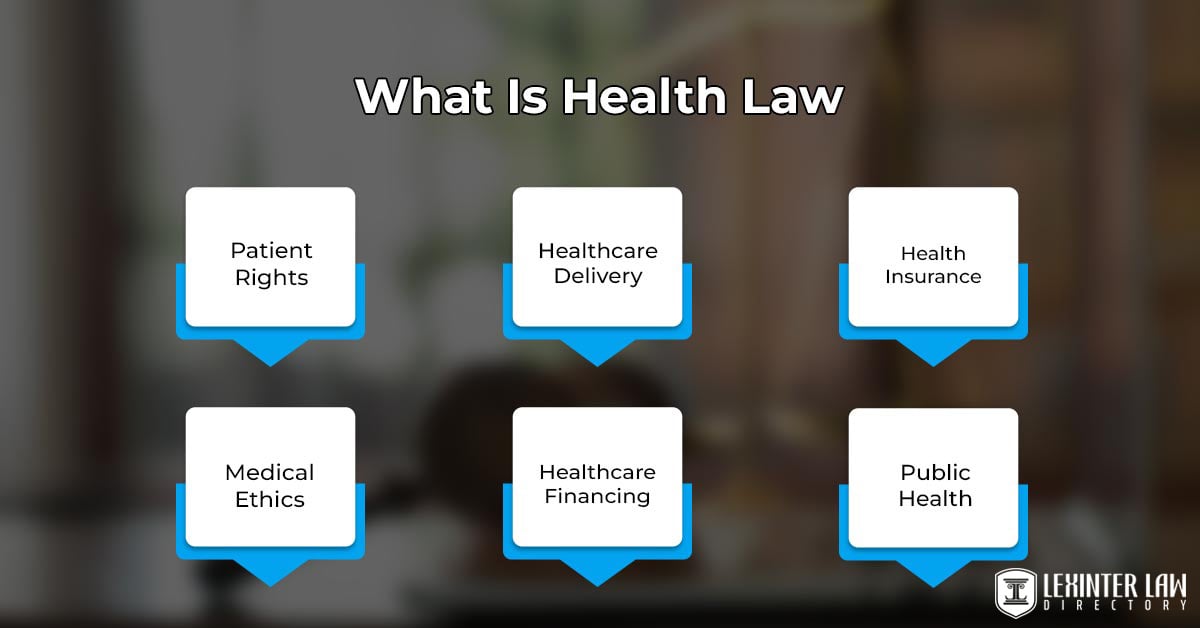
Health law is a specialized field of legal practice that encompasses a broad range of regulations, statutes, and ethical principles governing the healthcare industry and the delivery of healthcare services. Health law involves the legal framework that governs healthcare providers, institutions, patients, and the relationships and transactions within the healthcare system.
Law in Health addresses issues related to medical ethics, patient rights, healthcare organization and governance, healthcare financing and insurance, healthcare regulation, medical malpractice, and the intersection of law and medicine. Health lawyers, known as healthcare lawyers or health law attorneys, are legal professionals who specialize in providing counsel, advocacy, and representation in matters related to health law.
Health lawyers work to ensure that healthcare practices and policies are compliant with legal and ethical standards while advocating for the rights and interests of healthcare providers and patients within the complex landscape of healthcare regulation and delivery.
What Is The Importance Of Health Laws?
The importance of health laws lies in their capacity to protect patients’ rights, uphold healthcare quality, facilitate regulatory oversight, and provide ethical guidance within the healthcare sector. Health laws are essential for maintaining the trust, reliability, and effectiveness of the healthcare system, benefiting individuals and communities by ensuring access to safe, high-quality healthcare services.
Health laws are essential for patient protection. They establish a comprehensive framework of legal rights and responsibilities for patients, encompassing informed consent, privacy, access to medical records, and the right to receive appropriate and safe healthcare. Health law ensures that patients are treated with dignity, respect, and fairness, and that their healthcare decisions are made with full awareness and consent.
Health laws contribute to quality assurance within the healthcare industry. They help mitigate medical errors, reduce instances of medical malpractice, and ultimately enhance the safety and effectiveness of healthcare services by setting stringent standards and regulations. Health law not only safeguards patient well-being, but upholds the credibility and trustworthiness of healthcare providers and institutions.
Health laws provide a crucial framework for regulatory oversight. Government agencies and authorities use these laws to monitor and enforce compliance with healthcare standards, licensing requirements, and safety protocols. The oversight is vital in ensuring that healthcare facilities, professionals, and pharmaceuticals adhere to established norms, safeguarding public health, and minimizing the risk of substandard care.
Health laws address complex ethical dilemmas that frequently arise in the field of healthcare. They offer guidance and legal mechanisms for addressing issues such as end-of-life care, organ transplantation, research involving human subjects, and the protection of vulnerable populations. The ethical underpinning ensures that healthcare practices align with the values and principles of society.
What Is The Significance Of “Informed Consent” In The Realm Of Health Law?
The Significance of “Informed Consent” in The Realm of Health Law is the core ethical and legal concept that protects the autonomy, rights, and well-being of patients. Informed consent is the process by which healthcare providers, and doctors must tell patients about the nature, risks, benefits, and alternatives of a proposed medical treatment, procedure, or intervention. Patients must voluntarily and fully agree to or refuse the recommended course of action.
The idea of “informed consent” respects and strengthens individual autonomy and the right to make informed choices about one’s own body and health care. Informed consent makes sure that patients have all the knowledge they need to take an active role in their medical care. Informed consent gives them the power to make decisions that are in line with their values, preferences, and best interests.
Healthcare providers are held liable if they do not get informed permission from a legal point of view. Healthcare workers are required by law to get valid informed permission before doing any medical intervention. Healthcare workers are charged with medical malpractice, negligence, or even assault if they do not get informed permission, based on the situation. Consenting after being told what happened is an important part of the relationship between a doctor and a patient. Consenting helps build trust and openness in healthcare exchanges.
Giving informed permission keeps patients from getting hurt. Doctors help them make choices that reduce risks and increase benefits by telling patients about the risks and benefits of a medical procedure. Giving informed consent protects their physical and mental health and keeps them from feeling pressured into treatments they do not fully understand or agree with.
Informed consent is one of the most significant parts of health law because it is based on the ideas of autonomy, patient freedom, and openness in healthcare decision-making. Informed consent not only protects people’s rights, but it keeps doctors from doing things that are against the law. The concept of “informed consent” makes sure that healthcare workers put their patients’ best interests and well-being first. It helps build trust and ethics in the healthcare field.
How Is Medical Ethics Related To Health Law?
Medical ethics and health law are related in disciplines that intersect and mutually influence one another in the healthcare domain. Medical ethics furnishes the ethical underpinning for many of the principles and values embedded in health law. Ethical concepts such as patient autonomy, beneficence, non-maleficence, and justice serve as guiding beacons in medical ethics and health law. These principles shape healthcare providers’ decision-making processes and inform the development of healthcare laws and regulations, reinforcing a commitment to ethical healthcare practices.
One of the key areas where medical ethics and health law converge is in the notion of informed consent. Medical ethics mandates that healthcare practitioners must fully apprise patients of their treatment options and secure their voluntary consent. Health law translates these ethical directives into legal requirements, ensuring that informed consent is not only an ethical imperative but a legally binding obligation. The convergence serves to safeguard patients’ rights and autonomy while providing a clear legal framework for healthcare providers.
Civil law is a fundamental component of the legal system. Civil law plays a pivotal role in addressing medical ethics and health law issues. It primarily comes into play in cases involving professional liability and medical malpractice. Civil law furnishes a mechanism for patients to seek redress and compensation for harm or injuries incurred due to medical negligence or misconduct in situations where ethical standards are not met. Civil law sets legal standards and procedures for resolving disputes and claims about medical care, offering a structured framework for the application of ethical principles in a legal context.
Civil law governs contractual relationships within the healthcare sector, including agreements between patients and healthcare providers, and contracts involving healthcare institutions and insurers. These contracts frequently incorporate ethical considerations, such as patient confidentiality and rights, and are subject to legal enforcement through civil courts. Civil law provides the means for patients to assert and protect their rights, including seeking legal remedies if they believe their rights, privacy, or autonomy have been violated, aligning with the ethical principles that underscore patient dignity and well-being.
Medical ethics and health law collaborate to guide the practice of healthcare, ensuring that ethical values are upheld within a legally structured framework. Civil law plays a central role in the intersection of these two fields by addressing legal disputes, enforcing ethical standards, and safeguarding patients’ rights within the healthcare landscape as an integral component of the legal system.
What Are The Legal Procedures Involved In Addressing Cases Of Medical Malpractice?
The legal procedure involved in addressing cases of medical malpractice is to determine if a healthcare provider or institution deviated from the standard of care, resulting in patient harm. The legal procedure starts with the injured patient or their family consulting a medical malpractice attorney, who assesses the case’s merits.
A preliminary investigation follows once a formal complaint is filed against the responsible party, involving the gathering of medical records and consultation with medical experts. The other party responds after the defendant is served with the complaint, either admitting or denying the allegations.
The critical “discovery phase” follows, during which sides exchange information, depose witnesses, and consult expert witnesses. Settlement negotiations occur at any stage to resolve the case without a trial. The case proceeds to trial If not settled, where evidence is presented, and a verdict is reached by a judge or jury.
A judgment is entered during the post-trial, and either party appeals the verdict if they believe there were legal errors. The specific procedures and timelines vary by jurisdiction and experienced medical malpractice attorneys are crucial for navigating these complex cases effectively.
What Does The Health State Regarding Medical Information Privacy?
The health state regarding medical information privacy in the United States is primarily governed by the Health Insurance Portability and Accountability Act (HIPAA) of 1996. HIPAA is a federal law that establishes strict rules and standards to protect the privacy and security of individuals’ medical information, known as protected health information (PHI).
Healthcare providers, health plans, and healthcare clearinghouses must implement safeguards to ensure the confidentiality of PHI under HIPAA. Confidentiality of PHI includes restrictions on the disclosure of PHI without patient consent, the requirement to obtain written authorization for certain uses and disclosures, and the establishment of administrative, physical, and technical safeguards to secure electronic PHI (ePHI).
HIPAA provides individuals with the right to access their medical records, request corrections, and receive an accounting of disclosures. Individual states have additional privacy laws that further protect medical information, and they vary in their stringency, while HIPAA sets a national standard. The health state in the U.S. places a strong emphasis on safeguarding patient privacy and ensuring that healthcare entities handle medical information with the utmost care and confidentiality.
How Do Health Insurance Regulations Impact Access To Medical Services Under Health Law?
Health insurance regulations impact access to medical services under health law by the influence of several critical aspects of healthcare accessibility. Health insurance regulations dictate coverage requirements, mandating the types of medical services that insurance plans must include. Regulations in Health Insurance ensure that essential healthcare services, ranging from preventive care to hospitalization and prescription drugs, are accessible to individuals with insurance coverage. Health insurance regulations prioritize preventive care by requiring insurers to cover services such as vaccinations and screenings without cost-sharing for policyholders, incentivizing individuals to seek preventive services and improve their health.
These regulations emphasize network adequacy, compelling insurers to maintain a robust network of healthcare providers, including primary care physicians and specialists. The regulations safeguard policyholders’ access to a diverse range of medical services. Regulations prohibit discriminatory practices, particularly under the Affordable Care Act (ACA), which bars insurers from denying coverage or imposing higher premiums based on pre-existing conditions. Such provisions significantly enhance access to medical services by ensuring that individuals with chronic illnesses or health issues obtain coverage and receive essential care.
Health insurance regulations prescribe essential health benefits, encompassing services such as maternity care, mental health and substance use disorder services, and pediatric dental and vision care. Regulations in Health Insurance mandate that individuals purchasing insurance have access to comprehensive healthcare services. Regulations incorporate affordability measures, including income-based subsidies, which reduce the financial burden of premiums and out-of-pocket costs, enhancing access for low- and moderate-income individuals and families.
These regulations include consumer protections, such as limitations on annual and lifetime benefit caps and requirements for transparent communication about coverage and costs. Such safeguards help policyholders understand their coverage and rights, simplifying the process of accessing necessary medical services. Medicaid expansion, implemented in states that chose to expand the program under the ACA, has extended health insurance coverage to more low-income individuals, significantly broadening access to medical services for previously uninsured populations.
Health insurance regulations are pivotal in shaping access to medical services. They achieve it by prescribing coverage requirements, prioritizing preventive care, ensuring network adequacy, preventing discrimination, defining essential health benefits, addressing affordability, safeguarding consumers, and expanding Medicaid coverage. These regulations collectively contribute to establishing a healthcare system that offers equitable access to medical services for a diverse spectrum of individuals and communities.
How Does The FDA Regulate The Approval And Monitoring Of Drugs Under Health Law?
The FDA or Food and Drug Administration regulates the approval and monitoring of drugs under health law by involving stringent stages aimed at ensuring the safety and efficacy of pharmaceutical products. The FDA commences with preclinical testing in laboratories and on animals to assess a drug’s safety and potential effectiveness.
Pharmaceutical companies submit an Investigational New Drug (IND) application to the FDA to initiate human clinical trials following successful preclinical results. These trials, conducted in three phases, assess safety, efficacy, and side effects in human subjects under the supervision of physicians, researchers, and institutional review boards (IRBs).
Drug manufacturers submit a comprehensive New Drug Application (NDA) to the FDA once clinical trials are completed, providing extensive data on the drug’s safety, efficacy, manufacturing processes, labeling, and proposed usage. The FDA reviews the NDA meticulously, utilizing teams of medical, scientific, and regulatory experts.
The FDA approves if it determines that the drug’s benefits outweigh its risks upon a thorough assessment of clinical trial data, labeling, and risk-benefit analysis. The FDA allowing it to be marketed in the U.S. Post-approval, the FDA continues to play a vital role in monitoring drug safety and effectiveness through mechanisms like the Adverse Event Reporting System (FAERS).
Collaborating with organizations such as the American Health Lawyers Association (AHLA) helps address legal and regulatory complexities associated with drug safety, ensuring the highest standards of healthcare and legal compliance in the pharmaceutical industry. The FDA has the authority to take regulatory actions, including label modifications, safety alerts, or removal of a drug from the market, must safety concerns emerge after approval. The FDA’s rigorous regulatory process is instrumental in safeguarding public health by ensuring that drugs meet stringent safety and efficacy criteria before they reach the American public.
How Does Health Law Address The Practice Of Telemedicine And Its Legal Implications?
Health law addresses the practice of telemedicine and its legal implications by adapting to the evolving landscape of telemedicine, addressing its practice and associated legal implications to ensure quality healthcare delivery while safeguarding patient rights and safety.
Health law makes sure that patients get good care and that their rights and safety are protected. Telemedicine has become more popular, especially in cases like the COVID-19 pandemic, which is the use of technology to provide medical services from a distance.
Health law recognizes how important telemedicine is for giving people in underserved places more access to care. It talks about the practice of telemedicine by explaining what it is, how it is paid for, and who does it. Laws such as the Health Insurance Portability and Accountability Act (HIPAA) set rules about privacy and security. These rules make sure that patient information is kept safe during telemedicine sessions.
Health law has clarified liability issues, informed consent processes, and malpractice issues as a result of telemedicine’s legal implications. It sets rules for professional licensing across state lines. Health law lets healthcare workers offer telemedicine services to patients in other states, often through interstate compacts and waivers.
These rules help set up a regulatory framework that supports the growth of telemedicine while keeping patients safe and doctors legally responsible. Health law stresses how important it is to keep the same standard of care for telemedicine as for regular in-person care. It makes sure that patients get quality healthcare no matter how they get it. Health law tries to take advantage of telemedicine’s ability to improve access to healthcare while keeping legal and ethical standards in place for the delivery of remote healthcare services by addressing these issues.
What Are The Benefits Of Health Law?

The benefits of Health Law are listed below.
- Patient Protection: Health law establishes legal rights and safeguards for patients. Health law ensures that patients have the right to informed consent, privacy, and access to their medical records. These protections empower individuals to make informed decisions about their healthcare and protect their personal health information.
- Healthcare Rights: Health law protects the rights of vulnerable populations, including the elderly, disabled, and mentally ill. It ensures that these individuals receive appropriate care and are not subjected to discrimination or abuse within the healthcare system.
- Quality Assurance: Health law sets standards for healthcare quality and safety. It mandates regulations and guidelines for healthcare providers and institutions, reducing the risk of medical errors, negligence, and substandard care. It leads to improved patient outcomes and better healthcare.
- Ethical Framework: Health law provides a legal framework for addressing complex ethical dilemmas in healthcare, such as end-of-life decisions, organ transplantation, and medical research involving human subjects. It ensures that ethical principles like patient autonomy and beneficence are upheld.
- Insurance and Access: Health law includes provisions related to health insurance and access to care. Laws like the Affordable Care Act (ACA) have expanded access to insurance coverage and prohibited insurance companies from denying coverage based on pre-existing conditions.
- Research and Innovation: Health law governs medical research and innovation, ensuring that research involving human subjects follows ethical guidelines and legal standards. It regulates the approval and marketing of new drugs and medical devices, striking a balance between innovation and safety.
- Public Health Protection: Health law enables governments to respond to public health emergencies and outbreaks by implementing measures such as quarantine, vaccination, and contact tracing. It helps safeguard public health by controlling the spread of infectious diseases and protecting the population.
- Consumer Information: Health law requires healthcare providers and institutions to provide clear and accurate information to patients, allowing them to make informed choices about their healthcare. It includes information about treatment options, costs, and available resources.
- Regulatory Oversight: Health law grants government agencies the authority to regulate healthcare facilities, professionals, pharmaceuticals, and medical devices. Health law oversight helps ensure that healthcare practices adhere to established standards and that healthcare products are safe and effective.
What Legal Aspects Govern End-Of-Life Care?
The legal aspects governing end-of-life care are controlled by many laws, including federal, state, and local laws, ethical guidelines, and court decisions. These legal factors help them make important choices about their medical care and treatment as a person nears the end of their life.
Advance directives let people say how they want to be treated if they are unable to speak, such as living wills and permanent powers of attorney for health care. Do-not-resuscitate (DNR) orders state that a patient does not want cardiopulmonary resuscitation in certain situations. They are ruled by laws and rules. Physician Orders for Life-Sustaining Treatment (POLST) forms give detailed information about how a person wants to be treated to keep them alive.
State rules set up a hierarchy of surrogate decision-makers for people who do not make their own healthcare decisions and have not named a healthcare proxy or made advance directives. Palliative care and hospice services are controlled to make sure that people who are nearing the end of their lives get compassionate care that focuses on their symptoms. Ethical guidelines help doctors and nurses make hard choices about end-of-life care, which are put out by groups such as the American Medical Association and the American Nurses Association.
Laws about euthanasia and assisted suicide change from place to place and are subject to strict rules and safeguards. Legal requirements say that deaths must be reported and that death papers must be filled out correctly. Court decisions such as Cruzan v. Director, Missouri Department of Health, and Quill v. Vacco, which are considered landmark cases, have a big effect on problems like the withdrawal of life-sustaining treatment and assisted suicide.
These cases have changed the way the health law looks at end-of-life care. These legal aspects make up a framework for making choices about end-of-life care that tries to strike a balance between patient autonomy, ethical principles, and legal compliance. Doctors, patients, and their families get the right legal and moral advice to help them deal with these complicated and sensitive concerns.
How Do Mental Health Parity Laws Impact The Health Law?
The Mental Health Parity Laws impact the Health Law by addressing the equitable treatment of mental health and substance use disorder (MH/SUD) services in comparison to physical health services within the healthcare system. These laws try to get rid of differences in insurance coverage and access to care for mental health and drug abuse at the federal and state levels.
Health insurance companies must offer the same benefits for mental health and drug abuse as they do for physical health conditions under these rules. It means that insurance plans must cover mental health services, such as outpatient therapy, inpatient treatment, and prescription drugs, in the same way they cover medical and surgical services.
There are many ways that mental health parity laws affect people. These rules make it easier for people and communities to get help for mental health and drug abuse, which is very important for those who are struggling with these problems. These rules try to get rid of the financial barriers that have kept people from getting mental health care in the past by making everyone get the same coverage. It leads to better mental health and a better quality of life.
Mental Health Parity Laws help lessen the stigma that comes with mental health issues by making it clear that mental health is just as essential as physical health. The change in how people think about mental health issues makes it easier to talk about them, raise understanding, and make it more likely that people get help when they need it.
Compliance with Mental Health Parity Laws is a key part of health insurance control from a legal and regulatory point of view. Health plans must change how they handle coverage, documentation, and payment to comply with these rules. There are civil consequences, such as fines and jail time when not complying with the law.
Mental Health Parity Laws have a big effect on health law by making sure that everyone gets the same care for mental health and substance abuse. They make it easier for people to get care, reduce shame, and make sure that health insurance companies follow the law and treat mental health services and physical health services the same. It not only helps people who need mental health care, but it makes the healthcare system more complete and fair.
What Are The Legalities Surrounding Vaccine Mandates Within Health Law?
The legalities surrounding vaccine mandates within health law are listed below.
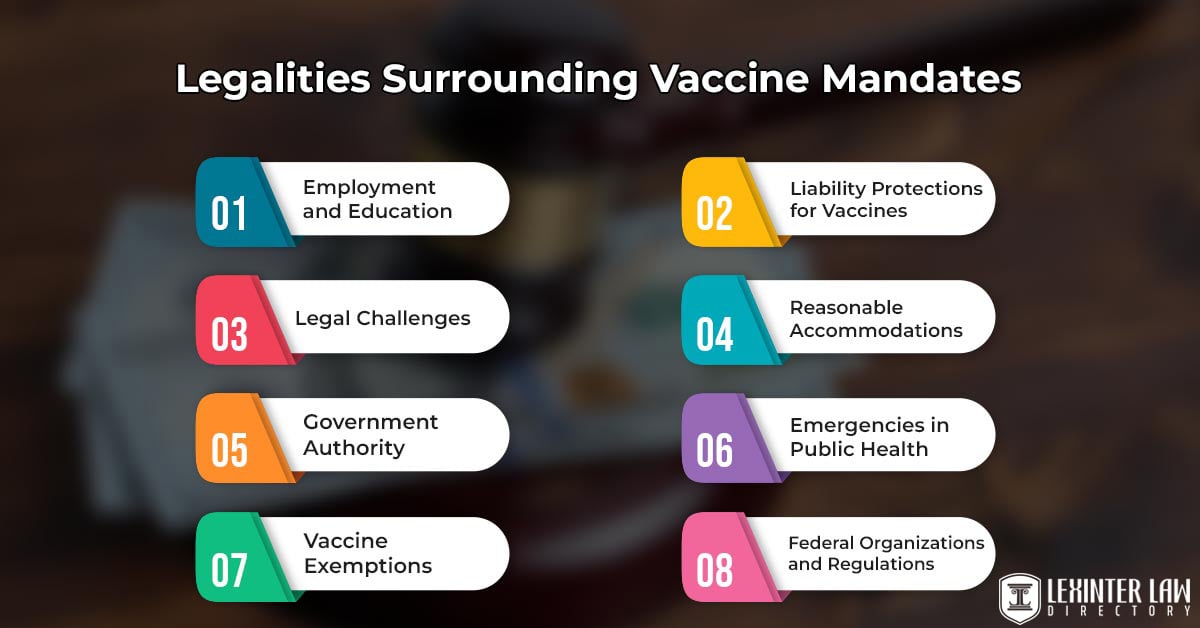
- Employment and Education: There are many places where vaccines are required, such as schools, hospitals, and some jobs. People have to get vaccinated as a condition of work, enrollment, or attendance if these laws are in place. Employers and schools have the legal right to implement such requirements, but they must take into account state and federal laws.
- Legal Challenges: Laws that require people to get vaccines are challenged in court. People or groups challenge mandates based on their right to personal freedom, their religious views, or other legal reasons. Courts have often weighed these cases against the government’s need to protect public health.
- Government Authority: The U.S. Constitution gives the states a lot of power to make rules about public health and safety. The rules include the ability to force people to get shots when there is a public health emergency. Agencies such as the Centers for Disease Control and Prevention (CDC) suggest vaccine requirements at the federal level, but it is up to the states to put them into place and make sure they are followed.
- Vaccine Exemptions: Most vaccine laws include exemptions for medical reasons or medical exemptions and for religious or philosophical reasons or nonmedical exemptions in some cases. The rules for these exemptions are different from one state to the next, and some states may have stricter rules for nonmedical exemptions.
- Liability Protections for Vaccines: The National Childhood Vaccine Injury Act (NCVIA) protects vaccine makers, healthcare workers, and people who give vaccines from being sued. The law set up the National Vaccine Injury Compensation Program (VICP), which gives people money if they get hurt because of a vaccine.
- Reasonable Accommodations: Some people have real health problems that make them unable to get vaccinated. Employers and schools are required to make reasonable accommodations for people with disabilities under the Americans with Disabilities Act (ADA) and related state laws. It includes letting people who do not get vaccinated make other plans.
- Emergencies in Public Health: States have more power to force people to get vaccines for the greater good of the public when there are emergencies in public health, such as pandemics. These steps are temporary and are challenged in court. Emergency vaccine orders have different legal powers and reach depending on where people live.
- Federal Organizations and Regulations: Vaccines are approved and recommended by the FDA and CDC, which are federal organizations. These organizations give advice and make rules about the safety and effectiveness of vaccines, which have an effect on the vaccine laws in each state.
What Do Healthcare Lawyers Do?
Healthcare lawyers focus on health law, which is a complicated area with many parts. Healthcare lawyers’ main job is to find their way through the complicated legal landscape of the healthcare industry. Lawyers in healthcare deal with a wide range of legal issues connected to healthcare delivery, regulation, compliance, and patient rights.
Healthcare lawyers provide important services in many key areas, such as regulatory compliance. Healthcare lawyers help healthcare providers and groups understand and follow federal and state healthcare regulations such as HIPAA, Medicare, and Medicaid. They help with licensing and certifying healthcare workers and facilities to make sure they meet the necessary qualifications and standards. There are guides on ‘How to Become a Health Lawyer: Essential Steps and Pathway to Success’ to meet the qualifications and standards of becoming a healthcare professional.
Healthcare lawyers help with significant deals in the healthcare sector, such as mergers, acquisitions, contract negotiations, and partnerships. They represent healthcare providers in cases of medical negligence, defend them against accusations of negligence, and protect their professional reputations.
Patient advocacy, developing ethics and compliance programs, healthcare litigation, protecting the protection of health information, and working with the government are some other important things that healthcare lawyers do. The knowledge of healthcare providers helps protect the legal rights of healthcare stakeholders, make sure that the law is followed, and uphold ethical standards. Healthcare lawyers make sure that patients get the safety and quality care they deserve in a healthcare system that is always changing.
What Legal Considerations Come Into Play Regarding Reproductive Rights?
The legal considerations that come into play regarding reproductive rights encompass a complex and multifaceted legal landscape. The problem of abortion rights is the most essential of these. Laws about how to get an abortion vary a lot from country to country, and even within the United States.
Laws about abortion range from making it easy to get an abortion to making it hard or making individuals wait. Roe v. Wade, a landmark U.S. Supreme Court case, said that a woman has a constitutional right to choose to have an abortion. However, later rulings have given states some power to regulate abortion.
Access to birth control is another important factor. Laws cover things like how birth control is covered by insurance and whether birth control is bought without a prescription. Important parts of reproductive rights law include sexual education in schools, parental rights and consent for minors seeking reproductive health care, assisted reproductive technologies, fertility preservation, and protections for health care providers who have religious or moral objections.
Privacy and confidentiality, equal treatment, and foreign agreements on human rights have a big impact on how reproductive rights are written into the law. The field is always changing because of legal and political debates, new laws, and the way people feel about reproductive health and family planning problems.
What Is The Right To Health Scope in International Health Law?
The right to health scope in International Health Law encompasses the notion that every individual is entitled to enjoy the highest attainable standard of physical and mental health. The right covers a wide range of things, such as access to preventive, curative, and palliative care, and treating the social factors that affect health, such as poverty, housing, nutrition, and access to clean water. Nondiscrimination and equality in healthcare, active participation in healthcare choices, and government accountability for upholding rights are important parts.
The right to health is based on the Universal Declaration of Human Rights, the International Covenant on Economic, Social, and Cultural Rights, and other international and regional human rights laws. States that sign these agreements have a legal duty to support, protect, and carry out the right to health. These tasks cover a wide range, from not doing things that make it harder to get healthcare to taking steps to make sure healthcare is available, easy to get to, and of good quality. People and groups use the law to get justice when their right to health is violated. For example, they file complaints with international human rights bodies or in local courts.
Human rights law in healthcare law is a subset of legal principles and international agreements that focus on safeguarding and promoting fundamental human rights in the context of healthcare and medical treatment. Human rights law is rooted in the belief that every individual has inherent rights that must be protected, respected, and fulfilled when it comes to their health and well-being.
The right to health has a big impact on how healthcare policies are made and carried out. It tells governments to give priority to healthcare access for disadvantaged groups, use resources wisely, and deal with social factors that affect health. It has a big effect on how foreign agreements are made and how organizations like the World Health Organization do their jobs. The right to health supports the idea of health equity. It means that governments have to work to get rid of differences in health care and make sure that everyone, no matter where they come from or what their circumstances are, has the chance to be healthy.
What Are Prevented By Healthcare Fraud And Abuse Laws?
The Prevented by Healthcare Fraud and Abuse Laws are listed below.
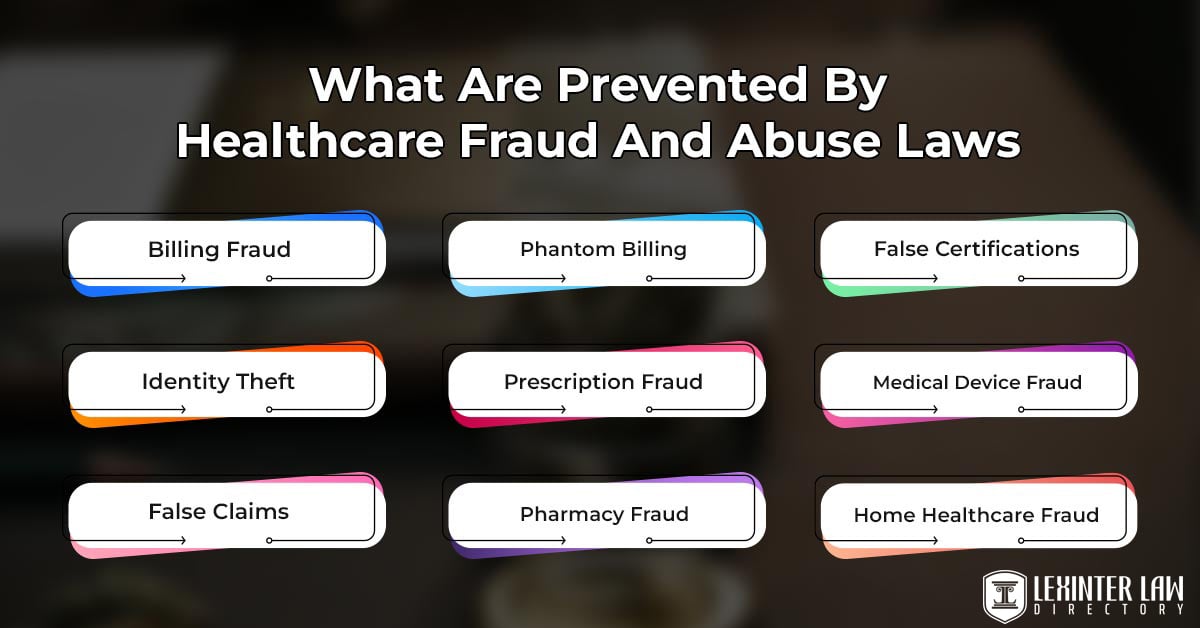
- Billing Fraud: Billing fraud includes things such as overbilling, upcoding, and unbundling. Upcoding means billing for a more expensive service than what was provided. Unbundling means billing separately for services that must be billed together. Such actions cause people to make false claims and cause healthcare programs to lose money.
- Identity Theft: Identity theft is against healthcare privacy laws and fraud laws to steal or use a patient’s personal or medical information for false reasons, such as getting medical services or prescription drugs.
- False Claims: False Claims are against the law to submit false claims for reimbursement, such as claims for services that were not done or were not medically required. It causes healthcare organizations and patients to lose money.
- Phantom Billing: Billing for services or procedures that were never done is called “phantom billing.” Healthcare fraud rules are meant to stop scams. It leads to false claims and costs healthcare programs more money than they need to.
- Prescription Fraud: Prescription fraud includes things such as making fake scripts, “doctor shopping” going to multiple doctors to get multiple prescriptions, and selling prescription drugs without a prescription. Prescription theft puts people’s health in danger and causes healthcare programs to lose money.
- Pharmacy Fraud: Healthcare fraud laws try to stop pharmacies from doing things that are against the law, such as filing false claims, giving out fake drugs, or getting kickbacks. It is to protect patients and healthcare programs.
- False Certifications: Making up certifications or paperwork for medical services or tools leads to false claims and possible violations of laws against healthcare fraud.
- Medical Device Fraud: Medical device theft is a type of fraud that happens when medical devices are made, sold, or billed dishonestly. Some examples are lying about how safe or effective a device is or billing for devices that were never given.
- Home Healthcare Fraud: Fraud in the home healthcare business, like billing for services that are not done or giving services that are not needed, hurts patients and costs money to healthcare programs.
- Kickbacks and Inducements: Healthcare fraud laws make it illegal to offer, pay, ask for, or receive kickbacks, bribes, or inducements in exchange for patient recommendations, services, or orders of medical equipment. These practices make it harder for doctors to make choices and cause healthcare costs to go up.

